The CDC defines Severe Maternal Morbidity (SMM) as 'unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to a woman's health.' These outcomes are largely preventable and are an important indicator of maternal health care quality. The CDC reports that SMM has steadily increased in recent years, and the consequences are wide-ranging, including detrimental effects on women's health, longer hospitalization stays, and increased medical costs. Measuring and tracking SMM is an important part of health surveillance that can help health care providers and policy makers pinpoint shortfalls in the health care system and prioritize maternal health.
This analysis used HCCI data to identify the CDC's 21 indicators of SMM in the ESI population and calculate rates of SMM per 1,000 births.
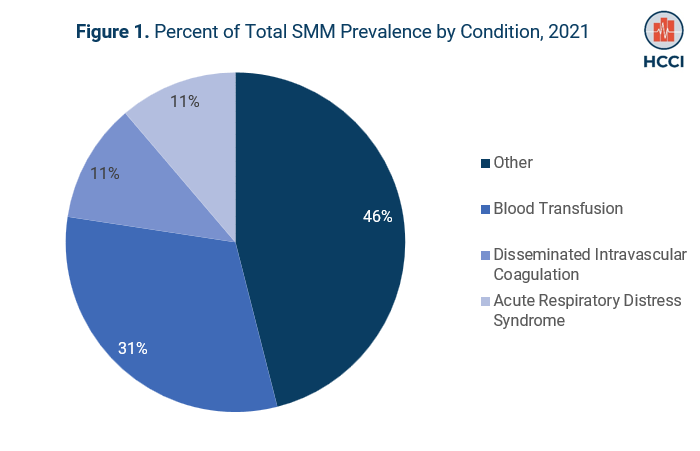
Of the CDC's SMM indicators within HCCI's data, blood transfusion was the most common (6.62 per 1,000 births), followed by disseminated intravascular coagulation (2.40 per 1,000 births), and acute respiratory distress syndrome (2.34 per 1,000 births).
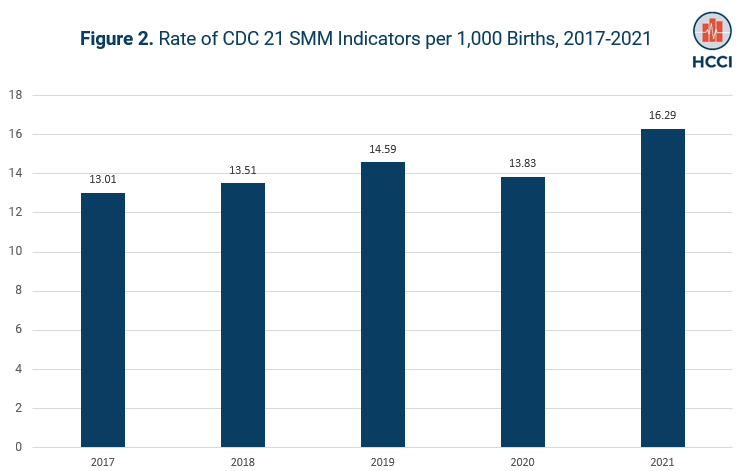
As shown in Figure 2, from 2017 to 2021, the SMM rate increased by 25%, with a nearly 18% increase from 2020 to 2021. In 2021, of all births that occurred in an inpatient setting, SMM affected about 16 out of every 1,000 births.
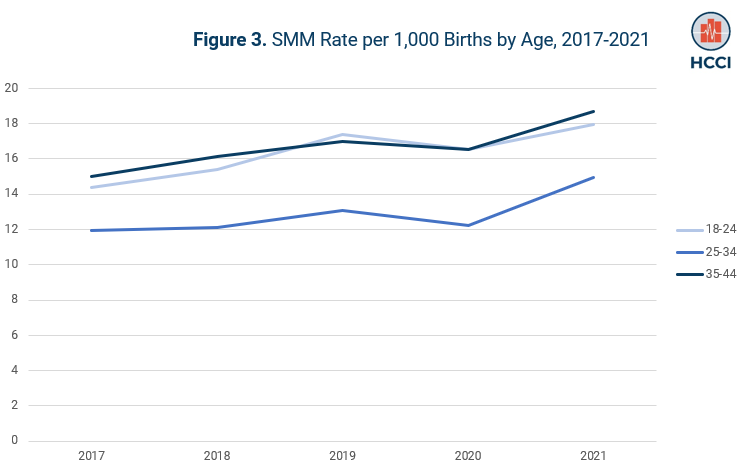
Among women ages 18-44 in this analysis, rates of SMM were highest among people aged 35-44 and 18-24. All age groups in this cohort experienced the same level of growth in SMM rates from 2017-2021. (Figure 3.)
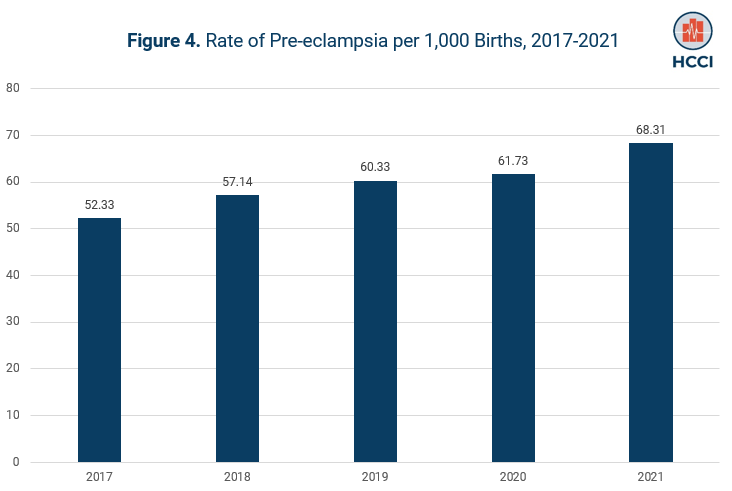
Previous research has included pre-eclampsia as an SMM indicator. Pre-eclampsia, high blood pressure during pregnancy, can lead to complications for the birthing person and baby and is estimated to occur in 5-8% of births. As shown in Figure 4, in 2021, pre-eclampsia occurred in nearly 68 out of every 1,000 births in HCCI's ESI data. The rate of pre-eclampsia has increased by approximately 30% from 2017-2021, with an 11% increase from 2020-2021.
Rates of pre-eclampsia were highest among birthing people aged 18-24, and people in the 25-34 age group experienced the largest growth in pre-eclampsia rates from 2017-2021.
This analysis is consistent with other reports of increasing rates of severe maternal morbidity and pre-eclampsia. Because private insurance pays for more than half of all births in the U.S., understanding trends in this population is an important bellwether for maternal health in the country. Future work should build on this to include people enrolled in Medicaid, which is responsible for covering more than 40% of births in the U.S., and to explore what is driving the trends over time.
Methods Note
We restricted our childbirth cohort to childbirth claims for females enrolled in ESI, ages 18-44. We identified childbirth claims as any inpatient claims with a vaginal delivery or C-section DRG code (Vaginal: 767, 774, 775, 796, 797, 798, 805, 806, 807, 768; C-Section: 765, 766, 783, 784, 786, 787, 785, 788). We assigned DRGs based on the diagnosis and procedure codes to which most spending was attributed. This methodology may exclude a small number of births where procedures occurred during the admission that were more expensive than the birth. We identified births with SMM as any childbirth claim that had an SMM diagnosis in any diagnostic position on the inpatient or corresponding professional claims.